What Art Can You Not Start With Viral Load 100000
- Research Article
- Open up Access
- Published:
Very high baseline HIV viremia impairs efficacy of non-nucleoside reverse transcriptase inhibitor-based ART: a long-term ascertainment in handling-naïve patients
Infectious Diseases of Poverty volume 9, Commodity number:75 (2020) Cite this commodity
Abstract
Background
Information technology is non completely clear whether a very high pre-therapy viral load (≥ 500 000 copies/ml) can impair the virological response. The aim of this study was to examine the influence of very loftier baseline HIV-RNA levels on long-term virological responses nether one type of regimen.
Methods
A retrospective study was performed based on data from two multicenter cohorts in China from January to November 2009, and from May 2013 to Dec 2015. Untreated HIV infected adults between 18 and 65 years former were recruited before receiving not-nucleoside opposite transcriptase inhibitor-based regimen. All patients had baseline HIV-RNA levels over 500 copies/ml, good adherence, and were followed for at least 24 weeks. Virological suppression was divers as the outset HIV-RNA < l copies/ml. Virological failure was divers as whatever of incomplete viral suppression (HIV-RNA ≥ 200 copies/ml without virological suppression within 24 weeks of treatment) and viral rebound (confirmed HIV-RNA level ≥ fifty copies/ml after virological suppression). Chi-square test, Kaplan–Meier analysis, Cox proportional hazards model and Logistic regression were used to compare virological response between each pretreated viral load stratum.
Results
A total of 758 handling-naïve HIV patients in People's republic of china were enlisted. Median follow-up time (IQR) was 144 (108–276) weeks. Past week 48, rates of virological suppression in 3 groups (< 100 000, 100 000–500 000 and ≥ 500 000 copies/ml) were 94.i, 85.0, and 63.8%, respectively (P < 0.001). Very loftier baseline HIV viremia over 500 000 copies/ml were found to be associated with delayed virological suppression (≥ 500 000 vs < 100 000, adjusted relative adventure = 0.455, 95% CI: 0.32–0.65; P < 0.001) as well as incomplete viral suppression (≥ 500 000 vs < 100 000, adjusted odds ratio [aOR] = 6.084, 95% CI: 2.761–13.407; P < 0.001) and viral rebound (≥ l 000 vs < 100 000, aOR = 3.671, 95% CI: 1.009–13.355, P = 0.048).
Conclusions
Very high levels of pre-treatment HIV-RNA were related with delayed efficacy of NNRTI-based ART and increased risk of handling failure. More than potent initial regimens should be considered for those with this clinical graphic symbol.
Background
As the chief treatment for HIV infected patients, the benefits of highly agile antiretroviral therapy (ART) in reducing mortalities past suppressing the plasma viral load to an undetectable level has been well established [1,ii,3]. However, poor virological responses to treatment were observed in certain patients, which may require prolonged treatment to achieve the expected virological suppression. There are occasions when patients even fail the primary regimen with absence of own resistance-associated mutations.
Virological response to ART could be related to several factors including historic period, sex, manner of manual, drug adherence, drug resistance, hepatitis virus coinfection, and pretreatment HIV-RNA levels [2]. Among the factors that may have an influence on the virological response to ART, the level of baseline HIV-RNA greater than 100 000 copies/ml before the start of treatment was proved an contained predictor of delayed virological suppression likewise as increased gamble of virological failure, leading to increased mortality in several studies [two, 4,5,6,vii,8]. A previous cohort study suggested that a very high pre-treatment viral load greater than 500 000 copies/ml significantly impairs the virological response. This study, even so, was express by diversified choice of regimen, as ritonavir-additional protease inhibitors (PI/r) was more frequently used in patients with higher baseline viral load due to its high barrier of drug related resistance [nine]. Another study confirmed the link betwixt very loftier baseline viral load and poor virological responses while some crucial factors were ignored, including treatment modifications and adherence [10]. Therefore, the role of a very high baseline HIV-RNA level in long-term virological responses to Art remains unclear, especially with certain types of regimens.
The combination of two nucleoside opposite transcriptase inhibitors (NRTI) + non-nucleoside opposite transcriptase inhibitor (NNRTI) has been recommended as the showtime-line handling until 2015, when integrase strand transfer inhibitor (INSTI) based regimen were established [11]. However, NNRTI-based regimens are withal widely used every bit the first-line treatment across centre- and low-income countries including Cathay, for the consideration of accessibility and cost-efficiency [12, xiii]. The aim of the present study was to examine the influence of very high baseline HIV-RNA levels on long-term virological responses to the regimen of 2NRTIs + NNRTI in a big cohort of HIV-infected patients.
Methods
Participants and study design
A retrospective report was performed based on two completed prospective multi-center accomplice in Cathay. Details of both cohorts accept been described in detail elsewhere [14, xv]. The data of patients in the two cohorts were collected from January to Nov 2009, and from May 2013 to December 2015. The cohorts included HIV-treatment naïve patients betwixt 18 and 65 years sometime. Recruited patients received Art and were followed regularly, when data including HIV-RNA levels, CD4 cell count, adverse furnishings and adherence were collected. In this study, patients were selected according to the following criteria: 1) available information of baseline HIV-RNA level and CD4 cell count; 2) 2NRTIs + NNRTI as their initial regimen; 3) baseline HIV-RNA over 500 copies/ml; 4) over 98% adherence to the treatment, assessed by self-report, i.eastward. patients reporting their missed doses from the final time of visit; 5) time of follow-upwardly longer than 24 weeks, to ensure plenty time for evaluating efficacy.
Information including age of diagnosis, sexual activity, fashion of transmission and clinical characteristics such equally HIV subtype, baseline HIV-RNA level, baseline CD4+ T cell count, planned regimen, year of ART initiation and co-infections including seropositivities of hepatitis B virus surface antigen (HBsAg) and hepatitis C virus antibody (HCV-Ab) were nerveless. Pre-treatment HIV-RNA levels were categorized equally < 100 000 copies/ml, 100 000 to 500 000 copies/ml and ≥ 500 000 copies/ml. Baseline CD4 cell count were categorized as < 100 cells/mm3, 100–199 cells/mm3, 200–350 cells/mm3 and > 350 cells/mmiii. Plasma HIV-RNA level and CD4 cell count at each follow-upwardly afterward the first of treatment (calendar week 12, 24, 48, 72, 96, 144, 192) were as well collected for analysis.
For the bachelor pre-treatment resistance information, we used the Genotypic Resistance Interpretation Algorithm – HIVdb Programme (HIVdb, Stanford University, Stanford, CA) to calculate penalization scores for relevant NRTI and NNRTI, and sequences were determined to be either susceptible (< 15, including potential depression-level resistance) or resistant (≥ 15; low-, medium-, or high-resistance).
The prospective cohorts in this written report had been approved by Institutional Review Board of Peking Union Medical College Hospital and complied the Principles of Proficient Clinical Practice and the Declaration of Helsinki. Patients were enrolled in the cohorts after informed consents were signed to provide their anonymized data for academic not-for-profit studies.
Endpoints
Definitions of virological suppression and virological failure differ betwixt different regions [xvi, 17]. The present study defined virological suppression equally the time bespeak when plasma HIV viral load was less than 50 copies/ml. Virological failure was defined as incomplete viral suppression (defined as HIV-RNA remaining ≥ 200 copies/ml without always achieving virological suppression by week 24 after the start of the handling) or viral rebound (defined as confirmed HIV-RNA level ≥ 50 copies/ml after virological suppression). Blips (an isolated HIV-1 RNA at to the lowest degree fifty copies/ml that is immediately preceded and followed by virological suppression) were excluded from patients who met the rebound definition, since it was not related with virological failure according to previous reports [18].
Statistical analyses
All statistical analyses were performed using the SPSS 24.0 statistical software packet (IBM Corporation, Armonk, NY) and GraphPad Prism version 8 (GraphPad Software, Inc., La Jolla, CA). Baseline demographic and clinical characteristics were summarized using medians (interquartile ranges [IQRs]), and frequencies (percentages). Chi-squared test was used in analyzing virological suppression charge per unit in three different groups. Kaplan-Meier curves were used to gauge the time and probability to achieve virological suppression. Multivariable Cox proportional hazard models were used to adapt for potential confounders and outcomes were expressed as ratio risk (RH) with confidence intervals of 95% conviction interval (95% CI). Patients were right-censored if they did not achieve virological suppression but stopped follow-up. Binary Logistic regression was used to evaluate the odds ratio (OR) to incomplete viral suppression and viral rebound. Factors with associations with P < 0.10 in univariate analysis were entered into the multivariable model. All tests of significance were 2-sided, with a P value < 0.05 indicating that an association was statistically pregnant.
Results
Demographic characteristics of the written report population
The study sample was based on 758 eligible pre-treatment HIV infected patients. Demographic and clinical characteristics of the included patients are shown in Tabular array 1. Patients were mainly male (565 [74.5%]), with a median age of 33 (24–71) years erstwhile. Regarding pre-handling HIV-RNA level, 27.8 and half-dozen.iii% of patients, showed viremia ranging between 100 000–500 000 copies/ml, and ≥ 500 000 copies/ml, respectively. Most selected patients (338 [44.six%]) had baseline CD4 jail cell count between 200 and 350 cells/mm3. The near commonly used regimen was tenofovir disoproxil fumarate (TDF) + lamivudine (3TC) + efavirenz (EFV) (517 [68.2%]). In those whose genetic testing were available, very few had significant resistance to their regimen (16/353 [4.5%]). The median follow-upwards time of the written report population was 144 (108–276) weeks.
Virological trajectories in patients with different levels of baseline HIV-RNA
Overall, 529 (69.viii%) of the patients in the cohort had achieved virological suppression past week 24, and 671 (89.7%) patients accomplished virological suppression by calendar week 48. At week 24, only xviii/48 (37.five%) patients with a baseline HIV-RNA over 500 000 copies/ml had achieved virological suppression, compared with 117/211(55.5%) in those with a baseline betwixt 100 000 and 500 000 copies/ml. Figure ane shows the percentage of patients that achieved virological suppression in different baseline level groups at week 12, 24, 48, 72 and 96. The rates of virological suppression in those with higher pretreatment viral load remained all the manner lower than those with lower pretreatment viral load except for the kickoff 12 weeks. At week 96, 718 (94.7%) patients nonetheless remained in the sample cohort, and the percentage of virological suppressed patients in three groups by rise baseline HIV-RNA levels were 88.6, 95.9 and 98.3%, respectively. Chi-foursquare analysis suggested all the difference in percentage betwixt each group at dissimilar time points were significant (P < 0.001). In addition, the cumulative Kaplan-Meier estimation showed a significantly lower probability of virological suppression for higher HIV-RNA categories (log-rank P < 0.001, Fig. 2). Subsequently the handling, the median CD4 prison cell count of all the patients in the cohort rose from 263 (165–245) cells/k3 at week 0 to 446 (319–545) cells/m3 at week 96. Table 1S shows the number of patients that remained in three groups and of those who achieved virological suppression in each follow-upwardly.
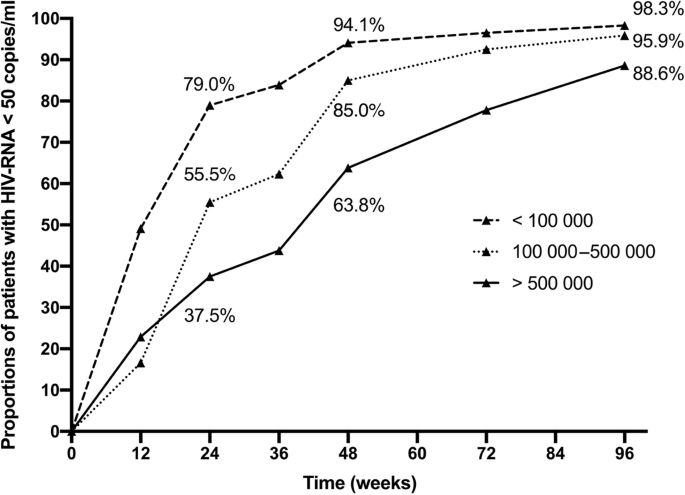
Per centum of patients based on baseline HIV-RNA level who had achieved virological suppression in unlike follow-upward. P < 0.001 on Chi-square analysis
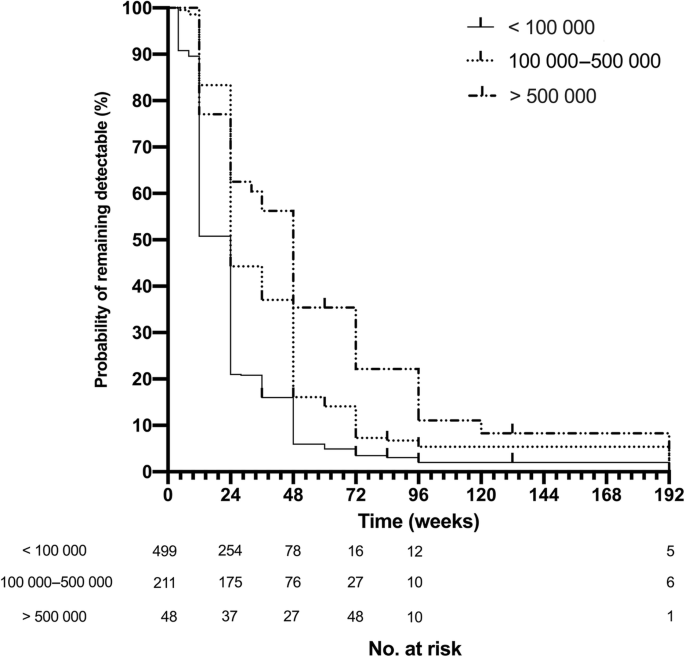
Kaplan–Meier curve of time to virologic suppression based on baseline HIV-RNA levels. Log-rank P < 0.001
Univariate and Multivariable Cox proportional gamble models were used to clarify factors associating with time to virological suppression (Table 2). Very high baseline HIV viremia over 500 000 copies/ml were found to exist independently associated with delayed virological suppression, subsequently adjusting for factors including sex, age, mode of transmission, HIV-subtype, pre-treatment CD4 cell count, sero-positivity of HBsAg and HCV-Ab (≥ 500 000 vs < 100 000, adjusted RH [aRH] = 0.455, 95% CI: 0.319–0.648; P < 0.001). Male person sex activity was shown to be another significant relevant gene of deterred virological suppression (male person vs female, aRH = 0.755, 95% CI: 0.622–0.916, P < 0.001). None of age, pre-handling CD4 cell count, fashion of transmission, HIV-subtype, pre-treatment resistance, initial regimen, sero-positivity of HBsAg of HCV-Ab was significantly associated with delayed virological suppression.
High baseline HIV-RNA is related to virological failure
In the sample accomplice, 71/758 (9.4%) patients had incomplete viral suppression, amidst whom 21/71 (30.0%) had never achieved virological suppression. 23/758 (iii.0%) patients had viral rebound, with 7/23 (thirty.four%) having additional blips, ane/23 (four.iii%) having severe agin effect and stopped the initial regimen in calendar week 48. Of these patients, three/94 (3.ii%) were resistant to their initial regimen that was afterward proved by genetic analysis.
Binary Logistic regression models were built to evaluate factors related to incomplete viral suppression or viral rebound (Tables iii and four). Afterward adjusting with covariates including age, sexual activity, HIV subtype, pre-treatment resistance, baseline CD4 level, sero-positivity of HBsAg or HCV-Ab, mode of transmission, odds ratio (OR) to incomplete viral suppression were significantly higher in patients with baseline HIV-RNA levels ≥ 500 000 copies/ml (≥ 500 000 vs < 100 000, aOR = 6.084, 95% CI: 2.761–13.407; P < 0.001). Afterwards excluding patients with viral blips, baseline HIV viremia over 500 000 copies/ml were plant to be independently associated with rebound (≥ 500 000 vs < 100 000, aOR = 3.671, 95% CI: 1.009–xiii.355; P = 0.048).
Discussion
As reported by many previous studies, including some large-calibration studies with over 100 000 participants, that baseline HIV viral load over 100 000 copies/ml is associated with longer time to virological suppression as well as increased incidence of viral rebound [six,vii,8], notwithstanding very few had addressed the impact of baseline viral load over 500 000 copies to virological effect of ART [9, 10]. The present study reports virological changes of 758 treatment-naive HIV-infected patients from two prospective accomplice in long-term follow-upwardly. Our written report demonstrates that patients with very loftier baseline HIV-RNA levels, particularly those of over 500 000 copies/ml, were significantly associated with delayed or incomplete virological suppression and increased occurrence of viral rebound on NNRTI-based regimens. In add-on, the declining RH of virological response following viral load stratum rising suggested a decreased response with increased baseline viral load may establish a continuum. Our findings from prospective cohorts, in combination with previous studies, further emphasized the influence of baseline HIV-RNA > 500 000 copies/ml on virological response based on NNRTI regimens.
INSTI-based ART, in specific dolutegravir (DTG)- or raltegravir (RAL)-based regimens have been recommended as the kickoff-line regimen in about adult countries [xvi, 17] for their higher efficacy, less adverse effects and better tolerance [19]. Even so, clinical and programmatic experience with INSTI in depression- and middle-income countries is express due to the relatively high cost [20]. Currently, NNRTI-based ART regimens such as TDF + 3TC + EFV are still recommended as culling commencement-line regimens co-ordinate to WHO guidelines [12] and are still commonly used in many developing countries [21]. In improver, DTG-based ART may not exist as cost-constructive equally EFV co-ordinate to studies in many countries [22, 23], presenting other problems if completely replacing the latter very soon. On the other hand, there has been some studies demonstrating that the virological efficacy of EFV is amend than NVP, as both-based regimen were used in this study [24]. We made additional comparison between the number of patients being treated with EFV or NVP based regimen and the proportion in their baseline viral load strata, and it was shown that there was no predilection of either drug in whatsoever viral load stratum (Chi-square exam, P = 0.896).
Recent guidelines take recommended starting Art every bit soon equally HIV infection is confirmed, regardless of HIV-RNA level or time of infection so as to become rapid suppression of viral load [16]. In the present study, just 37.5% of the patients with baseline HIV-RNA ≥ 500 000 copies/ml accomplished virologic suppression at week 24, much less than those with lower baseline HIV-RNA levels. This trend continued into 96 weeks of handling, though by week 96 the differences of virologically suppressed percentage in all three viral load strata were getting smaller, suggesting that virtually patients may accomplish virological suppression given long-term treatment. In this report, in patients who met the definition of incomplete suppression, only 21 never achieve virological suppression during their follow-ups, while the rest of them had their viral load suppressed to undetectable in more than 24 weeks. Even so, it should exist noted that all patients meeting the definition of incomplete suppression need to be evaluated as virological failure, equally delayed or incomplete virological suppression volition increase risks of opportunistic infections and secondary manual, and some of these patients may never achieve virological suppression under the current regimen. In add-on, we establish that high baseline HIV viral load was associated with increased risk of viral rebound, equally is consequent with previous studies [9]. The difficulty of NNRTI-based regimens in suppressing such high viral loads indicated that more potent initial regimens, such as INSTI-based regimen should be preferably considered for these patients for early and rapid suppression of viral loads.
In the nowadays study, male sex was found to be an independent risk factor of delayed virologic suppression in multivariate Cox proportional hazard assay but not significantly related to incomplete suppression or viral rebound. Nosotros made an boosted comparison of proportions of male and female patients in each viral load stratum, finding that there was no divergence in distribution of both sexes (Chi-foursquare test, P = 0.136). In sub-analysis within each HIV-RNA group, male person sex was still significantly related with postponed virological suppression (P = 0.004 for HIV-RNA > 100 000 copies/ml, and P = 0.011 for HIV-RNA < 100 000 copies/ml). The association between male sex and postponed virological suppression in this study is consistent with the result of one previous study [ten]. Some previous analyses showed similar antiretroviral efficacy in men and women [25,26,27,28], in terms of the per centum of virological suppression instead of survival time. Sex was non significantly relevant to incomplete suppression or viral rebound in our study either, but this may be due to limited number of cases. There are differences in pharmacokinetics and pharmacodynamics betwixt sexes due to differences in torso composition, sexual activity hormones, microbiome, genetic and immunological differences [29, 30], and the response to handling equally measured by CD4+ T cell count recovery has been reported to favor women [31]. Equally HIV-infected women enrollment were limited by the major route of transmission in many trials and observations [28] including this report, the office of sex activity in viral response needs to be further studied.
Positive HBsAg and HCV-Ab were not significantly relevant with virological response in the present study. Like conclusions accept been reached past previous studies [32,33,34], even so some recent studies suggested that positive HBcAb or HCV-Ab may have adverse effects on the virological response [35, 36]. However, all studies demonstrated that both hepatitis virus seropositivities tin can decrease the recovery rate of CD4 T cells [32, 34,35,36], and this was not referred in the nowadays study.
The present study has some limitations. Firstly, the 95% CI in analysis of high baseline HIV-RNA and virological failure was wide due to a relatively small number of failed cases, also as very high baseline HIV-RNA level (≥ 500 000 copies/ml) patients. In this analysis, even so, the OR of virological failure increased as nosotros raised the viral load stratum. The result would be more than convincing if more cases were included. Secondly, adherence in this report was assessed by self-report, which may be less accurate than other methods such equally chemist's shop refilling, electronic adherence monitoring device [37]. As the adherence may be overestimated hither, this might also have contributed to the delayed or incomplete virological response in these patients. Thirdly, profiles of pre-handling resistance and HIV subtype were not available for all patients in our written report. The rate of primary drug resistance in China was around 3.0–iv.32% [38]. We analyzed drug resistance in virologically failed patients and found transmitted drug resistance was not chief contributor for their handling failure. For those who had never accomplished virological suppression, in that location are several factors that can be attributed to: unreported inadherence, unsatisfying gastrointestinal absorption, drug-drug interactions, and acquired drug resistance [39], yet the verbal reason of failed virological suppression in these patients were not able to be ascertained in this report.
Conclusions
Our findings in this report support that very high pre-treatment HIV-RNA levels are associated with dumb virological response. Male sex activity was also constitute to be related to postponed virological undetectability. Patients with very loftier HIV-RNA levels, especially those with baseline RNA over 500 000 copies/ml may possibly need some stiff regimens as their initial treatment.
Availability of information and materials
Datasets used in this assay are available from the corresponding author upon asking.
Abbreviations
- 3TC:
-
Lamivudine
- AZT:
-
Zidovudine
- DTG:
-
Dolutegravir
- EFV:
-
Efavirenz
- ART:
-
Antiretroviral therapy
- HIV:
-
Human immunodeficiency viruses
- INSTI:
-
Integrase strand transfer inhibitor
- NVP:
-
Nevirapine
- NRTI:
-
Nucleoside reverse transcriptase inhibitor
- NNRTI:
-
Non-nucleoside reverse transcriptase inhibitor
- PI:
-
Protease inhibitor
- RH:
-
Relative hazard
- TDF:
-
Tenofovir disoproxil fumarate
- OR :
-
Odds ratio
- VS:
-
Virological suppression
- WHO:
-
World Wellness Organization
References
-
Hogg RS, Yip B, Kully C, Craib KJ, O'Shaughnessy MV, Schechter MT, et al. Improved survival among HIV-infected patients afterward initiation of triple-drug antiretroviral regimens. JAMA. 1999;160(5):659–65.
-
Egger Thou, May Grand, Chene Yard, Phillips AN, Ledergerber B, Dabis F, et al. Prognosis of HIV-one-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002;360(9327):119–29.
-
Palella FJ Jr, Delaney KM, Moorman Air-conditioning, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and bloodshed amongst patients with advanced human immunodeficiency virus infection. HIV outpatient study investigators. N Engl J Med. 1998;338(xiii):853–threescore.
-
Wood Due east, Hogg RS, Yip B, Quercia R, Harrigan PR, O'Shaughnessy MV, et al. College baseline levels of plasma homo immunodeficiency virus blazon 1 RNA are associated with increased mortality after initiation of triple-drug antiretroviral therapy. J Infect Dis. 2003;188(10):1421–5.
-
Wood Due east, Hogg RS, Yip B, Harrigan PR, Montaner JS. Why are baseline HIV RNA levels 100,000 copies/mL or greater associated with mortality after the initiation of antiretroviral therapy? J Acquir Immune Defic Syndr. 2005;38(3):289–95.
-
Woods Eastward, Hogg RS, Yip B, Moore D, Harrigan PR, Montaner JS. Impact of baseline viral load and adherence on survival of HIV-infected adults with baseline CD4 jail cell counts > or = 200 cells/microl. AIDS. 2006;twenty(8):1117–23.
-
Stephan C, Hill A, Sawyer W, van Delft Y, Moecklinghoff C. Impact of baseline HIV-i RNA levels on initial highly active antiretroviral therapy outcome: a meta-assay of 12,370 patients in 21 clinical trials. HIV Med. 2013;14(v):284–92.
-
Raffi F, Hanf M, Ferry T, Khatchatourian L, Joly V, Pugliese P, et al. Affect of baseline plasma HIV-1 RNA and time to virological suppression on virological rebound according to first-line antiretroviral regimen. J Antimicrob Chemother. 2017;72(12):3425–34.
-
Santoro MM, Armenia D, Alteri C, Flandre P, Calcagno A, Santoro M, et al. Impact of pre-therapy viral load on virological response to modern first-line HAART. Antivir Ther. 2013;18(7):867–76.
-
Di Biagio A, Rusconi S, Marzocchetti A, Signori A, Schiavetti I, Bruzzone B, et al. The role of baseline HIV-ane RNA, drug resistance, and regimen type as determinants of response to first-line antiretroviral therapy. J Med Virol. 2014;86(10):1648–55.
-
EACS Guidelines version 8.0, Oct 2015 http://www.eacsociety.org/files/guidelines_8.0-english-revised_20160610.pdf. Accessed 19 Jun 2020.
-
Earth Health System. Updated recommendations on first-line and second-line antiretroviral regimens and post-exposure prophylaxis and recommendations on early babe diagnosis of HIV: interim guidelines. Supplement to the 2016 consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Geneva: World Health Organisation; 2018 (WHO/CDS/HIV/18.51). Licence: CC Past-NC-SA 3.0 IGO. https://apps.who.int/iris/bitstream/handle/10665/277395/WHO-CDS-HIV-18.51-eng.pdf?ua=1. Accessed 19 Jun 2020.
-
AIDS and Hepatitis C Professional Grouping, Club of Infectious Diseases, Chinese Medical Association;Chinese Middle for Disease Control and Prevention. Chinese guidelines for diagnosis and treatment of HIV/AIDS (2018). Zhonghua Nei Ke Za Zhi. 2018;57(12):867–84.
-
Luo Fifty, Wang N, Yue Y, Han Y, Lv Due west, Liu Z, et al. The furnishings of antiretroviral therapy initiation time on HIV reservoir size in Chinese chronically HIV infected patients: a prospective, multi-site cohort study. BMC Infect Dis. 2019;nineteen(1):257.
-
Li T, Guo F, Li Y, Zhang C, Han Y, Lye West, et al. An antiretroviral regimen containing 6 months of stavudine followed past long-term zidovudine for first-line HIV therapy is optimal in resource-express settings: a prospective, multicenter study in China. Chin Med J. 2014;127(ane):59–65.
-
EACS Guidelines version nine.i, October 2018. 2018. http://www.eacsociety.org/files/2018_guidelines-9.1-english.pdf. Accessed nineteen Jun 2020.
-
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Apply of Antiretroviral Agents in Adults and Adolescents with HIV. U.s.: Department of Health and Human being Services; 2019. Available at https://files.aidsinfo.nih.gov/contentfiles/lvguidelines/AdultandAdolescentGL.pdf. Accessed xix Jun 2020.
-
Fleming J, Mathews WC, Rutstein RM, Aberg J, Somboonwit C, Cheever LW, et al. Low-level viremia and virologic failure in persons with HIV infection treated with antiretroviral therapy. AIDS. 2019;33(thirteen):2005–12.
-
Kanters S JJ, Zoratti One thousand, Forrest J, Humphries B, Campbell J. Web Addendum B. Systematic literature review and network meta-assay assessing first-line antiretroviral treatments In: Updated recommendations on outset-line and second-line antiretroviral regimens and post-exposure prophylaxis and recommendations on early infant diagnosis of HIV: interim guidelines. Supplement to the 2016 consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Geneva: World Health Organization; 2018 (WHO/CDS/HIV/xviii.25). Licence: CC By-NC-SA three.0 IGO.
-
Vitoria Grand, Ford N, Clayden P, Pozniak AL, Hill AM. When could new antiretrovirals be recommended for national treatment programmes in low-income and center-income countries: results of a WHO think tank. Curr Opin HIV AIDS. 2017;12(iv):414–22.
-
Peng S, Tafazzoli A, Dorman E, Rosenblatt L, Villasis-Keever A, Sorensen S. Toll-effectiveness of DTG + ABC/3TC versus EFV/TDF/FTC for first-line treatment of HIV-1 in the U.s.. J Med Econ. 2015;eighteen(10):763–76.
-
Pialoux G, Marcelin AG, Cawston H, Guilmet C, Finkielsztejn L, Laurisse A, et al. Price-effectiveness of dolutegravir/abacavir/lamivudine in HIV-1 handling-naive (TN) patients in France. Expert Rev Pharmacoecon Outcomes Res. 2018;18(1):83–91.
-
Peng S, Tafazzoli A, Dorman E, Rosenblatt 50, Villasis-Keever A, Sorensen S. Price-effectiveness of DTG+ABC/3TC versus EFV/TDF/FTC for starting time-line treatment of HIV-1 in the United states of america. J Int AIDS Soc. 2014;17(4 Suppl 3):19605.
-
Cain LE, Phillips A, Lodi South, Sabin C, Bansi L, Justice A, et al. The outcome of efavirenz versus nevirapine-containing regimens on immunologic, virologic and clinical outcomes in a prospective observational written report. AIDS. 2012;26(13):1691–705.
-
Currier J, Averitt Bridge D, Hagins D, Zorrilla CD, Feinberg J, Ryan R, et al. Sex-based outcomes of darunavir-ritonavir therapy: a unmarried-group trial. Ann Intern Med. 2010;153(6):349–57.
-
Squires KE, Immature B, Santiago L, Dretler RH, Walmsley SL, Zhao HH, et al. Response by gender of HIV-1-infected subjects treated with abacavir/lamivudine plus atazanavir, with or without ritonavir, for 144 weeks. HIV AIDS (Auckl). 2017;9:51–61.
-
Squires K, Bekker LG, Katlama C, Yazdanpanah Y, Zhou Y, Rodgers AJ, et al. Influence of sex/gender and race on responses to raltegravir combined with tenofovir-emtricitabine in treatment-naive human being immunodeficiency virus-1 infected patients: pooled analyses of the STARTMRK and QDMRK studies. Open Forum Infect Dis. 2017;four(ane):ofw047.
-
Soon GG, Min M, Struble KA, Chan-Tack KM, Hammerstrom T, Qi K, et al. Meta-analysis of gender differences in efficacy outcomes for HIV-positive subjects in randomized controlled clinical trials of antiretroviral therapy (2000-2008). AIDS Patient Care STDs. 2012;26(8):444–53.
-
Matthews LT, Giddy J, Ghebremichael Thousand, Hampton J, Guarino AJ, Ewusi A, et al. A risk-factor guided approach to reducing lactic acidosis and hyperlactatemia in patients on antiretroviral therapy. PLoS One. 2011;vi(four):e18736.
-
Scully EP. Sex differences in HIV infection. Curr HIV/AIDS Rep. 2018;xv(2):136–46.
-
Gandhi RT, Spritzler J, Chan E, Asmuth DM, Rodriguez B, Merigan TC, et al. Upshot of baseline- and treatment-related factors on immunologic recovery after initiation of antiretroviral therapy in HIV-1-positive subjects: results from ACTG 384. J Acquir Immune Defic Syndr. 2006;42(iv):426–34.
-
De Luca A, Bugarini R, Lepri AC, Puoti M, Girardi Due east, Antinori A, et al. Coinfection with hepatitis viruses and outcome of initial antiretroviral regimens in previously naive HIV-infected subjects. Curvation Intern Med. 2002;162(eighteen):2125–32.
-
Chun HM, Mesner O, Thio CL, Bebu I, Macalino G, Agan BK, et al. HIV outcomes in hepatitis B virus coinfected individuals on HAART. J Acquir Immune Defic Syndr. 2014;66(2):197–205.
-
Marcus JL, Leyden WA, Chao CR, Xu 50, Quesenberry CP Jr, Tien PC, et al. Differences in response to antiretroviral therapy by sex and hepatitis C infection condition. AIDS Patient Care STDs. 2015;29(7):370–eight.
-
Malagnino V, Cerva C, Maffongelli G, Teti Eastward, Foroghi Biland L, Cesta Due north, et al. HBcAb seropositivity is correlated with poor HIV viremia control in an Italian cohort of HIV/HBV-coinfected patients on first-line therapy. Sci Rep. 2019;ix(one):11942.
-
Portocarrero Nunez JA, Gonzalez-Garcia J, Berenguer J, Gallego MJV, Loyarte JAI, Metola L, et al. Impact of co-infection past hepatitis C virus on immunological and virological response to antiretroviral therapy in HIV-positive patients. Medicine (Baltimore). 2018;97(38):e12238.
-
Orrell C, Cohen K, Leisegang R, Bangsberg DR, Wood R, Maartens G. Comparison of half-dozen methods to guess adherence in an Art-naive accomplice in a resource-poor setting: which best predicts virological and resistance outcomes? AIDS Res Ther. 2017;14(1):20.
-
Su Y, Zhang F, Liu H, Smith MK, Zhu L, Wu J, et al. The prevalence of HIV-i drug resistance among antiretroviral treatment naive individuals in mainland Communist china: a meta-analysis. PLoS One. 2014;ix(ten):e110652.
-
McCluskey SM, Siedner MJ, Marconi VC. Direction of virologic failure and HIV drug resistance. Infect Dis Clin North Am. 2019;33(3):707–42.
Acknowledgements
We thank the participants for their contributions to this study. We also give thanks Dr. Evelyn Hsieh for coordinating in the design of the study.
Funding
The study was supported by the National Cardinal Technologies R&D Program for the 13th Five-Twelvemonth Plan (Grant No. 2017ZX10202101), the National Fundamental Technologies R&D Programme for the 12th 5-Year Plan (Grant No. 2012ZX10001003–001), the National Key Technologies R&D Program for the 11th Five-Year Programme (Grant No. 2008ZX10001006–001), and the CAMS Initiative for Innovative Medicine (CAMS-I2M: 2017-I2M-ane-014). The funding bodies played no office in the design of the study, data collection, data analysis, interpretation of information, or writing of the manuscript.
Author information
Affiliations
Contributions
SC acquired, analyzed, interpreted the data and drafted the manuscript. XJS, YLL, HZL, XPT, TZhang, MZ, YH, SHH, MW, YZL, SBH, YL, JL conducted the clinical trial and acquired the clinical data in the accomplice. YH, TZhu provided back up for HIV-RNA measurement and coordinated in the design of the written report. WC coordinated in the design of the written report and revised the manuscript critically. TSL designed the study, interpreted the information and obtained funding. All authors participated in the manuscript review and approved the final version every bit submitted to Periodical of the International AIDS Lodge.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article was based on secondary data from two previous prospective studies with all identifying data removed. Patients were enrolled in the cohorts after informed consents were signed to provide their anonymized data for academic not-for-profit studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest related to this study.
Supplementary data
Additional file one: Table 1S.
Number of patients that achieved virological suppression and number of patients that remained in the cohort in each follow-upwards checkpoint.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution iv.0 International License, which permits use, sharing, adaptation, distribution and reproduction in whatsoever medium or format, as long every bit you give appropriate credit to the original author(south) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the commodity'southward Artistic Commons licence, unless indicated otherwise in a credit line to the material. If material is non included in the article'due south Artistic Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you volition need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/past/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zippo/i.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and Permissions
Near this commodity
Cite this article
Chen, S., Han, Y., Song, XJ. et al. Very high baseline HIV viremia impairs efficacy of not-nucleoside opposite transcriptase inhibitor-based ART: a long-term ascertainment in handling-naïve patients. Infect Dis Poverty 9, 75 (2020). https://doi.org/ten.1186/s40249-020-00700-8
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s40249-020-00700-8
Keywords
- HIV
- Viral load
- Baseline RNA
- Antiretroviral therapy
- Treatment outcome
- Virologic response
butlinellostaid1943.blogspot.com
Source: https://idpjournal.biomedcentral.com/articles/10.1186/s40249-020-00700-8